Professor Karen Canfell is a member of a working group of international experts convened by the International Agency for Research on Cancer (IARC) to review and assess all available studies of current methods for cervical cancer screening in terms of their effect on cervical cancer incidence and mortality. A Special Report published in The New England Journal of Medicine summarises the studies reviewed and presents the conclusions of the Working Group.
The detailed assessments will be published as Volume 18 of the IARC Handbooks of Cancer Prevention. Given the major advances in the field, this new evaluation offers an important update to the landmark 2005 Handbook on cervical cancer screening.
Cervical cancer is the second most common cancer type and the second most common cause of cancer death in women of reproductive age (15–44 years) worldwide. The highest incidence and mortality rates are generally observed in countries with the lowest values of the Human Development Index. Yet cervical cancer is largely preventable through both vaccination and screening for precursor lesions, with appropriate follow-up and treatment.
“Evaluations of the current screening methods in terms of their impact on cancer incidence and mortality will play a key role in helping to develop efficient public health policies to fight this preventable disease,” says Dr Béatrice Lauby-Secretan, Deputy Head of the Evidence Synthesis and Classification Branch at IARC.
In 2018, WHO called for a global initiative to eliminate cervical cancer as a public health problem. The evaluations from IARC Handbooks Volume 18 have been used as a basis to update the WHO Guideline for Screening and Treatment of Cervical Pre-cancer Lesions for Cervical Cancer Prevention.
“We reviewed and evaluated the evidence related to the efficacy and effectiveness of different cervical screening methods. HPV testing was shown to be more effective and a better balance of benefits versus harms when compared to other approaches,” Professor Canfell said.
“Some countries have already transitioned to primary HPV testing for cervical screening. In Australia, HPV testing has helped put us on track to becoming the first country to eliminate cervical cancer by 2028,” Professor Canfell added.
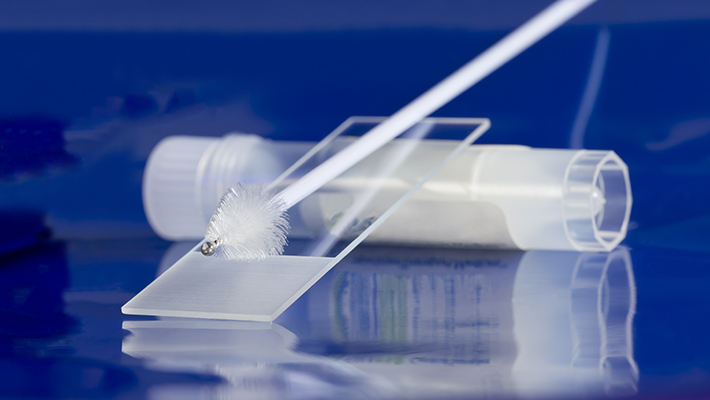
Transitioning to HPV screening, as well as being a more effective screening approach, has also enabled a new option for self-collection of the test. This week, Australia has taken another major step on the way to eliminating cervical cancer, with the announcement of changes to the National Cervical Screening Program (NCSP) that will provide the option for all people eligible for cervical screening to collect their own screening sample from next July. Funding self-collection for all program participants will be a game-changer for cervical cancer elimination in Australia.
“Participation is significantly lower in disadvantaged groups such as Indigenous women and other communities, and in individuals experiencing socioeconomic barriers to organised screening. A universal option to use self-collection will give these people more choice and control in the screening process.
“Research shows that self-collection is a safe and effective way to increase program participation, especially in the populations where we know screening rates are lower.”